Holistic Communication in Healthcare
Communication is a vital and very rewarding part of work in the Care sector. It has a big part to play in supporting someone with their physical, social, emotional and spiritual needs. Doing so, however, can often present challenges. Someone with a cognitive impairment (e.g. as a result of dementia, a head injury, or a stroke) may find it hard to communicate with us, and we may find it challenging to communicate in return.
Here are some examples of communication difficulties that can be associated with having a cognitive impairment:
- A difficulty coming up with the words they want to say, or using filler words like “thing” or “whatsit” instead
- Likely to repeat things that they have just said or things other people have said
- Tending to digress or go off on a tangent
- Difficulty understanding abstract language or phrases (e.g. “Rome wasn’t built in a day”; “it’s raining cats and dogs”)
- Problems understanding even single words
- Losing track of what they are saying
- Their speech may make little sense because they use the wrong words or sounds
- Resorting to/preferring non-verbal communication (e.g. nodding, pointing, but also agitation, striking out)
- Difficulty sticking to social “norms” in communication, such as interrupting others, not turn-taking and difficulty reading non-verbal cues (e.g. body language/facial expressions).
The list above refers to difficulties with language and the processing/production of words and sounds, however, there may be other “barriers” making communication more difficult:
- Sensory impairments - poor eyesight affects ability to use eye contact, poor hearing may mean listening to verbal communication is tricky
- Memory difficulties may mean that a person strongly believes that they are living at a different point in time from reality (e.g. they may believe they need to get back home before they collect their children from school)
- Environment - is it a busy or noisy place?
- What time of day is it? What would your own communication abilities be like if you were tired or had just woken up?
One theory is that people with dementia and other cognitive difficulties typically have a Lowered Stress Threshold which means that their levels of stress can build up more quickly than cognitively healthy people. Lots of things can contribute to stress levels, and any or all of them could impact on someone’s ability to communicate effectively with others.
Someone you work with may only present with one or two of these difficulties, or there could be problems with lots of these. Regardless of how many problems there are, it is important to know which ones you are likely to see, and how to work with them. The word holistic is often used in care planning, i.e. looking at the whole picture of someone as a person within themselves, who they are in their environment and social setting. This idea can certainly be applied to how we communicate with a person.
How can I improve my communication?
- Think about the environment - could you have a conversation somewhere quieter, less busy, more comfortable, or can you improve the current situation by, for example, turning down the TV/radio?
- Think about sensory issues - is the person’s hearing aid in/working properly? Can they see you?
- Think about physical health - if a person was in pain then how might they communicate that?
- Are you up to date with the individual, specific communication needs of this person? Check their care plan for current strategies, e.g. does this person prefer/respond best when using visual communication aids (symbols, pictures) alongside words?
- Are you speaking/communicating clearly enough with them? Are you being patient and giving them time to process what you have said? Are you close enough, loud enough, have you used their name to get their attention?
- Think about what you say - Are you using concise, short sentences? Could you use a simpler word and avoid jargon?
What if current strategies in someone’s care plan are not working?
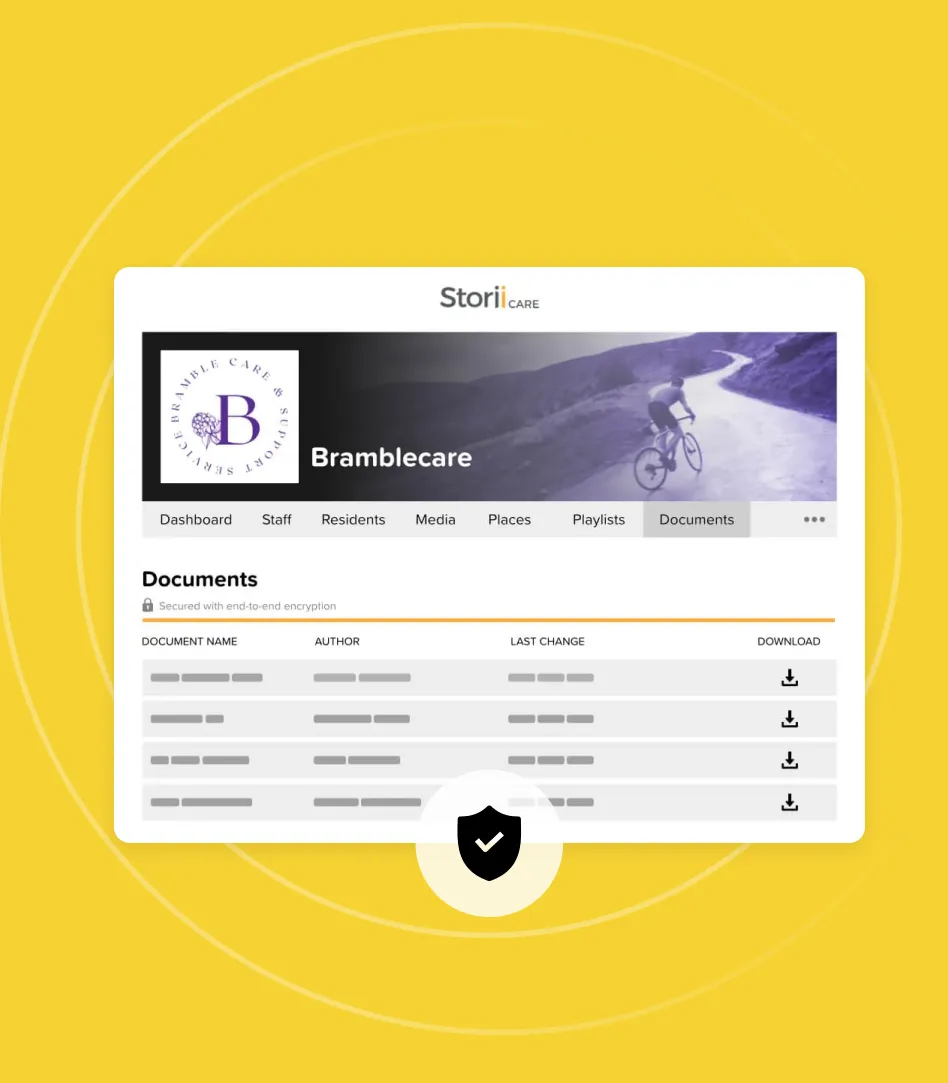
People’s needs change over time and may vary depending on how physically or mentally well they are at a given time. If a previously useful or successful strategy is no longer proving helpful, then it is likely time to review that person’s care plan. Switching to an electronic care plan will make it easier to amend care plans quickly and efficiently. However, when making changes to a care plan, it is also important to take a person-centred approach and collaborate with the person wherever possible and with the involvement of appropriate senior staff and relevant professionals. Try and discuss the issue respectfully with others in your team, and see if they are having similar difficulties. Most importantly of all, never give up on communication with someone, sometimes a bit of creative thinking can uncover new possibilities.



.png)
.png)
.png)